What are 4 steps in revenue cycle?
 What are 4 steps in revenue cycle?" />
What are 4 steps in revenue cycle?" />The Role of Medical Coding
Medical coding serves as a crucial component in the healthcare revenue cycle, acting as a bridge between healthcare providers and payers. It involves the translation of clinical documentation into standardized codes used for billing and insurance purposes. These codes reflect the services rendered, diagnoses made, and procedures performed. Accuracy in coding is essential, as it directly affects reimbursement rates and compliance with regulations. Errors in coding can lead to claim denials or delayed payments, significantly impacting a healthcare organization's financial stability.
The process of medical coding requires a keen understanding of both medical terminology and coding systems, such as ICD, CPT, and HCPCS. Coders often work closely with healthcare professionals to ensure that every aspect of patient care is accurately documented and translated into the correct codes. This collaboration ensures that providers receive appropriate compensation for their services while maintaining compliance with federal guidelines. Effective medical coding not only facilitates timely and accurate reimbursements but also supports the overall efficiency of the revenue cycle.
Importance of Accurate Medical Coding
Accurate medical coding serves as the backbone of the healthcare revenue cycle. It ensures that healthcare providers receive appropriate reimbursement for the services rendered. Mistakes or inaccuracies in coding can lead to claim denials, delayed payments, and potential loss of revenue. Furthermore, insurance companies rely heavily on these codes to assess the necessity and appropriateness of the care being billed. A single error can create rippling effects, cascading through the entire revenue cycle.
In addition to financial implications, proper coding is crucial for compliance with regulations and reporting standards. Incorrect codes can result in audits, fines, or legal action, putting healthcare organizations at risk. The integration of accurate coding also contributes to better data collection and analysis, aiding in overall operational efficiency. High-quality coding helps in identifying trends and improving the delivery of care, ultimately enhancing patient outcomes.
Revenue Cycle Metrics
Revenue cycle metrics are essential for assessing the effectiveness and efficiency of the financial processes within healthcare organizations. These metrics help identify areas of improvement and optimize operations. Metrics such as days in accounts receivable, claim denial rates, and cash collections can provide insights into the financial health of a practice. Tracking these indicators allows administrators to make informed decisions that can enhance revenue generation.
Regularly monitoring revenue cycle metrics enables healthcare providers to spot trends and adapt to changing circumstances. Analyzing the performance of billing and collections team is vital in ensuring timely payments. By understanding the data behind the revenue cycle, organizations can address bottlenecks and implement strategies that fortify their financial stability. Engaging with these metrics is not just a routine task; it is fundamental to sustaining profitability and growth.
Key Performance Indicators to Monitor
Monitoring key performance indicators (KPIs) is essential for evaluating the efficiency and effectiveness of the revenue cycle. These metrics provide insight into various aspects such as claim denial rates, days in accounts receivable, and collections as a percentage of net revenue. Tracking these indicators allows healthcare organizations to identify trends, make informed decisions, and implement necessary improvements to optimize their financial performance.
Regular analysis of KPIs helps organizations uncover areas requiring attention. By focusing on metrics like patient satisfaction scores and payment posting accuracy, leaders can assess operational effectiveness and enhance service delivery. Continuous monitoring also fosters a culture of accountability, motivating staff to strive for excellence in their roles, thereby positively impacting the overall revenue cycle.
Common Revenue Cycle Challenges
Organizations in the healthcare sector often face significant obstacles in managing their revenue cycles effectively. One prevalent challenge is the increasing complexity of insurance claims. As rules and regulations evolve, healthcare providers must stay current with coding guidelines, payer requirements, and compliance standards. This shifting landscape can lead to billing errors and delays in reimbursements, thereby affecting cash flow.
Another common issue arises from insufficient communication between departments. Fragmented processes hinder seamless information transfer, resulting in incomplete or inaccurate patient data. This lack of coordination not only contributes to operational inefficiencies but can also lead to slow claim resolutions and customer dissatisfaction. Ensuring that all stakeholders are aligned is crucial for optimizing revenue cycle performance.
Identifying and Overcoming Obstacles
Revenue cycle processes can often face several obstacles that hinder efficiency and profitability. Common challenges include issues with patient registration, claim denials, and inadequate follow-up on unpaid claims. Staff training and resource allocation play a pivotal role in addressing these barriers. When teams are well-versed in the intricacies of coding and billing, the likelihood of errors diminishes, increasing the chances for successful claim submissions.
Overcoming obstacles requires a proactive approach. Implementing technology solutions can streamline many processes, reducing manual errors and improving data accuracy. Regular audits help identify persistent issues within the revenue cycle, providing insights for corrective actions. Fostering a culture of continuous improvement enables health care organizations to respond swiftly to emerging challenges, ensuring that the revenue cycle remains robust and efficient.
FAQS
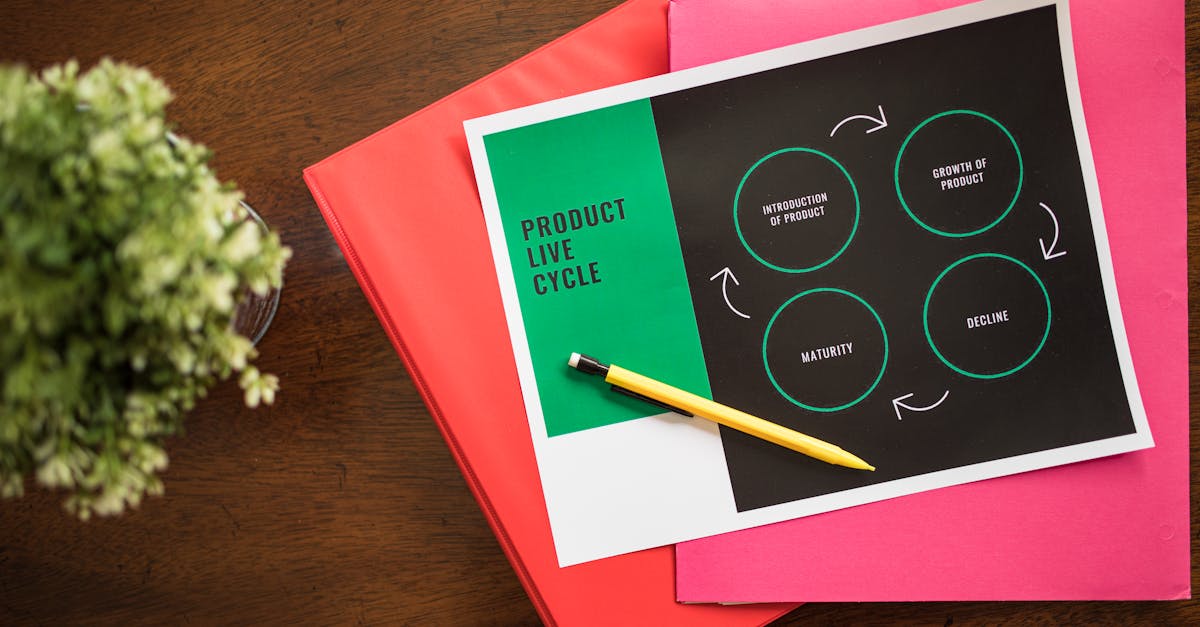
What are the four main steps in the revenue cycle?
The four main steps in the revenue cycle typically include patient registration, charge capture, claims submission, and payment posting.
Why is accurate medical coding important in the revenue cycle?
Accurate medical coding is crucial because it ensures that healthcare providers receive proper reimbursement for the services rendered, helps in minimizing claim denials, and maintains compliance with healthcare regulations.
How can revenue cycle metrics help healthcare organizations?
Revenue cycle metrics help healthcare organizations by providing insights into financial performance, identifying inefficiencies, and enabling data-driven decisions to improve overall revenue management.
What are some common challenges faced in the revenue cycle?
Common challenges in the revenue cycle include claim denials, billing errors, slow payment processes, and issues with patient eligibility verification.
What are key performance indicators (KPIs) to monitor in the revenue cycle?
Key performance indicators to monitor in the revenue cycle include days in accounts receivable, net collection rate, claim denial rate, and patient collection rate.
Related Links
revenue cycle outsourcingWhat is revenue cycle outsourcing?
What is the revenue of outsourcing?
What is the trend in outsourcing RCM services?